Do you have eating, drinking or swallowing difficulties?
Advice for people living with swallowing difficulties (Dysphagia) and their carers




Hello...
In 2020, MEAAP partnered with the Northern Health & Social Care Trust (NHSCT), in The Community Foundation Northern
Ireland (CFNI)’s Community Innovators Programme, funded by the Hospital Saturday Fund and the Department for
Communities.
The team’s aim was to support those living with swallowing difficulties in the community to better self-care. The result of this process is ‘Hard to Swallow’, a resource and campaign, designed in partnership with local Older People, health charities and Health & Social Care
professionals.
Its aim is to support our community and raise awareness of swallowing difficulties. The information on this website has been
compiled with support from the NHSCT.
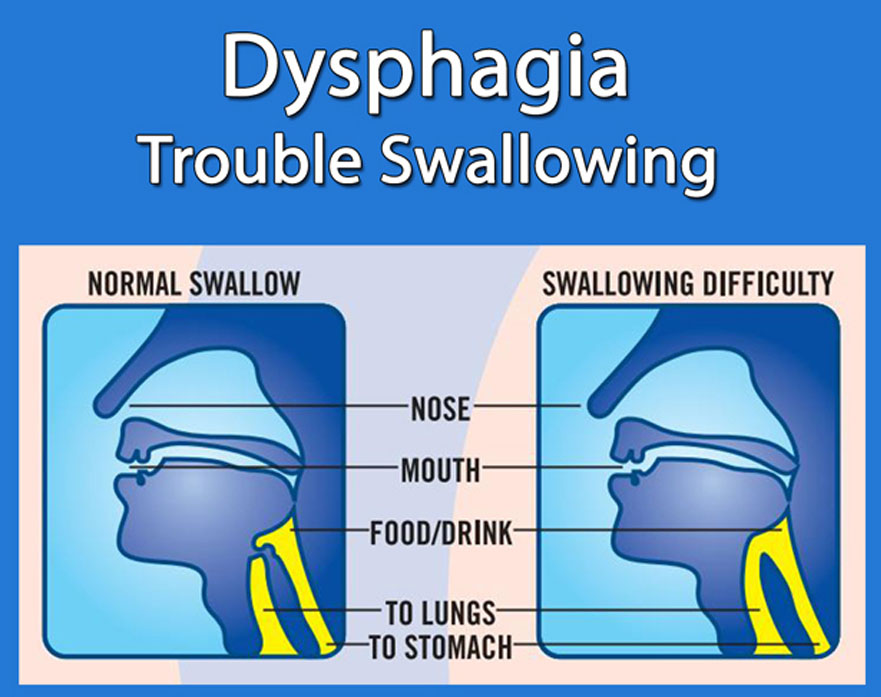
What is Dysphagia?
Research has shown that 16 – 23% of the general population have difficulties eating, drinking or swallowing, rising to 27% of those over 76 years.
Dysphagia (pronounced dys – fay – juh) is the medical term used when a person has difficulty eating, drinking or swallowing.
Difficulties with eating, drinking or swallowing can affect people at any stage in life.
Some people with dysphagia have problems swallowing certain foods or liquids, while others cannot swallow at all.
Dysphagia can improve, remain the same or get worse over time, depending on the cause.
Why does it happen?

Dysphagia can affect a wide variety of people and can occur as result of aging, frailty or following recovery from an illness. Some medical conditions can cause dysphagia e.g. conditions which affect the nervous system such as dementia, stroke, head injury, Parkinson’s disease, multiple sclerosis and motor neurone disease.
People with other conditions such as head and neck cancer,
cerebral palsy, learning disabilities and some mental health
conditions may also experience dysphagia.
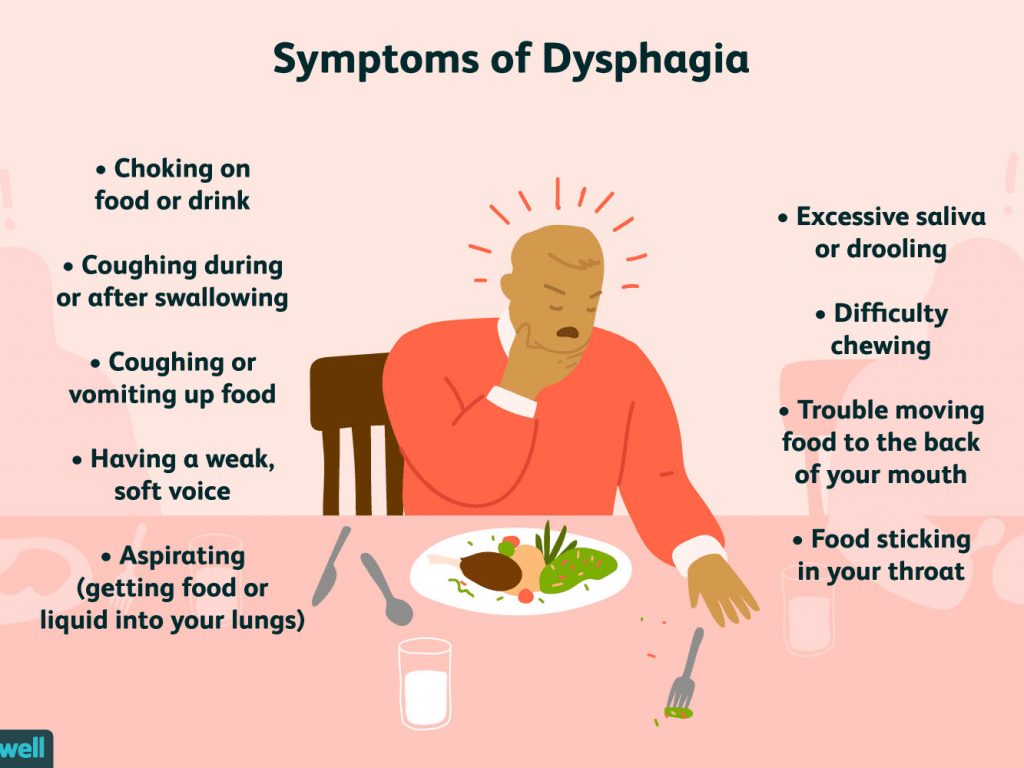
What are the signs of dysphagia?
You may notice one or more of the following signs:
• Coughing or choking during or after meals or drinks*
• Frequent chest infections – not accompanied by symptoms of the cold*
• Change in voice quality during or after eating and drinking – e.g. ‘gurgly’ or wet sounding voice*
• Change in breathing when eating and drinking e.g. wheezy, shortness of breath or gasping for air*
• Change of colour in the face when eating or drinking*
• Pieces of food found inside the person’s mouth after eating*
• High risk behaviours when eating and drinking e.g. cramming food in the mouth, not chewing food, holding food in the mouth, eating or drinking very quickly*
• Difficulty controlling food or liquid in the mouth
• A person reporting pain when swallowing or increased swallowing difficulties
• Difficulty managing own saliva
* Text adapted with permission from the Public Health Agency
What problems can Dysphagia lead to?
The serious physical health risks and complications of dysphagia include:
• Increased risk of choking
• Aspiration (when food, fluid or other material go into the lungs, which can lead to chest infections or aspiration pneumonia)
• Dehydration from drinking less
• Increased risk of other infections such as urinary tract infections
• Poor nutrition from eating less, which may lead to weight loss
• Loss of dignity, independence and potential for social isolation
• Admission to hospital or increased time in hospital
Dysphagia can also affect your quality of life because it may prevent you from enjoying meals and social occasions.
It is essential to speak to your GP or another health care professional if you, or someone you care for, is having difficulty swallowing or notice any signs of dysphagia. Your GP may refer you to:
A Speech & Language Therapist (SLT)
A Speech & Language Therapist assesses eating, drinking
and swallowing difficulties and may suggest ways to make
food and drinks easier and safer to swallow.
This may include advice about:
• changing the texture/thickness of food or drinks
• certain high risk foods to avoid
• swallowing exercises
In the Northern Health & Social Care Trust you can also contact the Speech & Language Department directly to ask for advice and discuss whether you might need an assessment.
A Dietitian
A dietitian can assess diet, nutritional & fluid intake and weight. They can provide you with advice on how to cook and prepare your meals to best meet the eating, drinking and swallowing recommendations made by your SLT.
A Specialist
Your GP may also refer you to a specialist doctor/consultant
e.g. Gastroenterology, ENT (Ear, Nose & Throat) – if further
tests are need
Making the most out of mealtimes
The following sections contain some general advice for individuals, and their families, who are experiencing eating, drinking and swallowing difficulties, to help you to ensure you are eating and drinking enough and to make mealtimes more enjoyable.
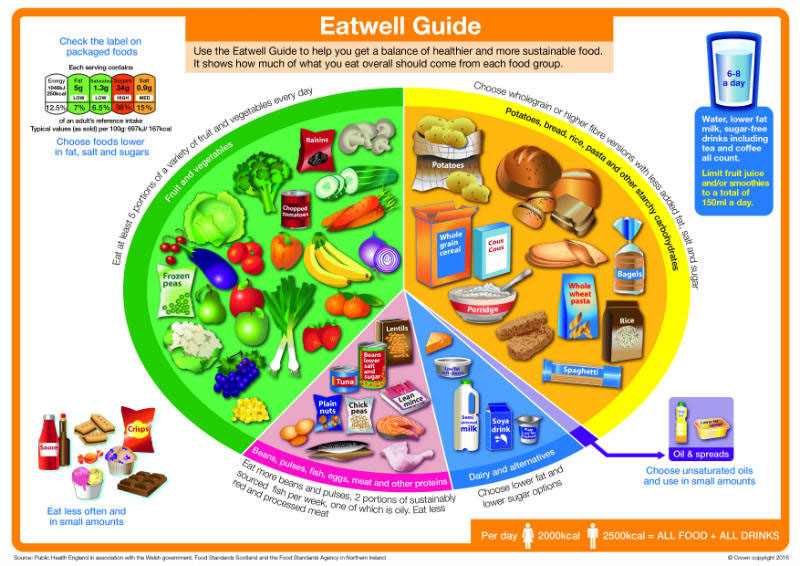
Ensuring a balanced diet
Often people find they eat less because they are anxious about choking; therefore, meals can take much longer to eat and are less enjoyable. There may also be certain foods you feel you are unable to eat safely so you may have less variety in your diet.
In order to get all the nutrition you need, ensure you eat foods from each of the food groups in the ‘Eatwell Guide’.
The Guide shows how much of what we eat should come from each food group to achieve a healthy, balanced diet. The advice in the Guide applies to most healthy adults.
Some foods may not be suitable for you personally or you may need to change how they are prepared or cooked before you eat them. A dietitian can give you personalised advice.
Older adults should note that weight loss is not a normal part of aging. If you or someone you are caring for is losing weight unintentionally, contact your GP.
If you are unintentionally losing weight or you have any
special dietary requirements, or medical needs, you may
need to speak to a registered dietitian to get advice on how to
adapt the ‘Eatwell Guide’ to meet your individual needs. You
can request a referral via your GP.
If you have been advised to follow a therapeutic diet for a medical condition, consult your dietitian for individualised advice.
What are modified texture foods / drinks?
People with dysphagia who have been assessed by a Speech and Language Therapist may be advised to change the texture of their food and/or drinks to make them easier and safer to swallow.
For some people, this could mean their food should be pureed or soft and cut into bite-sized pieces. For others this could mean adding a thickening powder to their drinks. The advice you receive may help you to feel that you can enjoy eating and drinking again.
Drinking enough with swallowing difficulties
People may drink less if they are worried about choking. Not drinking enough can cause dehydration, which can result in poor health. Dehydration may lead to:
• being thirsty
• feeling tired or lightheaded, reduced memory and
concentration
• low blood pressure
• having a dry mouth, lips or eyes
• dark yellow and strong-smelling urine, passing very little urine, and increased risk of urinary tract infections
• constipation
• increased risk of falls
How much do I need to drink each day?
You should aim to drink 6-8 large glasses or mugs (around2 litres) per day, but more if it is hot or you have been more active. Water, squash/diluting juice, minerals, fruit juice, milk, tea & coffee all count towards your fluid intake.
Tips to improve your fluid intake
• Have a drink beside you – take small sips
• Choose foods which have a high-water content e.g. thick soups, sauces or milky puddings such as custard or yoghurt
• Try drinks that are naturally thicker (smoothies or milkshakes)
• Try keeping track of how much you drink – some reusable drinks bottles have amounts marked
• Set an alarm to remind yourself to have a drink
What else can I do?
The first thing to do is to seek advice from a health care professional. If you have done this, and you are waiting for an appointment, or for the results of any tests, the following may help to make eating and drinking safer and mealtimes more enjoyable:
Position
• Make sure you sit fully upright – ideally try to remain sitting upright for 30 minutes after your meal
• Don’t lean to one side and do not tilt your head backwards
• Before swallowing, lower your chin towards your chest to reduce the chance of food/ drink going down the wrong way
During Meals
• Take small mouthfuls of foods and drinks
• Eat slowly. Chew your food extremely well and allow extra time to eat and drink
• Only take a drink when you have swallowed your food and mouth is clear
• Make sure each mouthful is swallowed properly before taking the next – it may be necessary to swallow at least twice after every mouthful to make sure everything has gone down
• Don’t try to talk while eating or drinking
• Small, frequent meals may be easier to manage
General Tips
• Ensure you are fully alert when eating and drinking
• Avoid distractions at mealtimes e.g. TV, music (you may be more likely to choke if you are focusing on something else)
• Make sure your mouth is empty after eating.
• Avoid using spouted beakers or straws unless specifically recommended by a speech & language therapist
• Fizzy drinks and very cold drinks may stimulate swallow sensation
If you are still struggling to drink enough each day, please speak to your GP.
High Risk Foods
Until speaking to a Speech and Language Therapist, you may wish to avoid some foods that are more difficult to chew or swallow, such as:
• tough meat
• boiled or chewy sweets
• soup with bits and chunks
• breakfast cereals that are not smooth/one consistency
• fruit and vegetables with skins or stringy bits
• crumbly foods e.g. pastry, biscuits
• hard or dry foods e.g. nuts, raw vegetables
Other Tips
• Remove skin, bones, gristle or hard bits when preparing meat, fish and poultry
• Vegetables that can be cooked until they are soft may be easier to swallow
• Floury potatoes, like Maris Piper, make smoother mash
• Hard pulses, like beans & peas, can be pureed
• Brown rice, risotto and short grain rice are easier to masher puree with liquid
• Soft and overcooked pasta will be easier to mash or puree
• Slow cooking cuts of meat such as; poultry thighs & legs or beef/pork shanks or cheeks, will result in softer, tender meat
• Poach fish instead of frying
• Items such as a potato ricer, sieve and hand blender can be useful to help remove lumps from foods
• Avoid using jars of baby food – the quantity, nutritional
content and taste is not appropriate for adults
Making food tasty
• Foods with stronger flavours can make swallowing easier
• Herbs, spices & condiments improve how food tastes
• Adding butter, sugar or cream to foods or drinks can improve the taste
• When food turns cold it can be less appetising. Try serving food on a warm plate or in thermal bowls and mugs
• Attractively presented food will stimulate the appetite
• Pureeing an entire meal is less appetising than if you puree each food separately
Eating Out

Just because someone has a swallowing difficulty, doesn’t mean they can’t still enjoy eating out or going to family gatherings.
It may make the experience easier if you plan ahead.
You could:
• Request a table in a more private part of the restaurant
• Let staff know that you may take a little longer to finish your meal
• Request a copy of the menu, or access it online, to allow you more time to choose your meal
• Let the restaurant / your host know of your requirements in advance
• If you use any particular crockery or cutlery – bring these with you
What can I do if I have difficulty swallowing medication?
Most types of pills are designed to be swallowed whole.
Chewing, breaking, or crushing them can change how the medication is digested and absorbed into the body. This change can affect the way a medication works and increase the chance of side effects.
Those with trouble swallowing medications should speak to their doctor and/or pharmacist for advice or to ask for different forms of medications e.g. liquid forms.
NEVER cut or crush tablets, open capsules or thicken medicines without advice from your pharmacist or GP.

How can I keep my mouth clean if I have swallowing difficulties?
Mouth care (Oral care) is important for everyone, even if you wear dentures or are fed via a tube. Mouth care is especially important if you have swallowing difficulties. Poor mouth care can lead to pain, gum disease and tooth loss. For people with swallowing difficulties, poor mouth care can increase the risk of chest infections and aspiration pneumonia.*
Keep your mouth clean and healthy by:
• Brushing your teeth (or dentures) twice a day for two minutes*
• Use a smear of low foaming toothpaste e.g pronamel / Oranurse on a dry tooth brush*
• Clean the whole mouth tongue / teeth / gums*
• Spit out toothpaste, do not rinse*
• If you are helping, stand behind the person tilting their head slightly forward to reduce the risk of swallowing residue or toothpaste*
If you are at increased risk of choking, seek further advice from a dentist*
What should I do if someone is choking?
1. Shout for help
2. Cough it out – encourage them to cough and remove any obvious obstruction from their mouth

3. Slap it out – if coughing fails to work, you need to give five sharp slaps on the back

4. Squeeze it out – If back blows fail to clear the obstruction, give five abdominal thrusts

If the blockage has not cleared, call 999 or 112 for emergency help straight away. Repeat five back blows and five abdominal thrusts until help arrives.
Where can I find more information?
General information
You can learn more about eating, drinking and swallowing
difficulties from the following websites:
NHS
www.nhs.uk/conditions/swallowing-problems-dysphagia/treatment/
Northern Health & Social Care Trust
www.northerntrust.hscni.net/services/speech-languagetherapy/dysphagia-2/
Public Health Agency
www.publichealth.hscni.net/publications/dysphagia-resources
The Eatwell Guide
More detailed information about healthy eating and the ‘Eatwell Guide’ can be found online at
www.nhs.uk/live-well/eat-well/the-eatwell-guide/
Modified Texture Diets
The International Dysphagia Diet Standardisation Initiative (IDDSI) is used to describe the texture of foods and thickness of drinks. More information can be found on the IDDSI website.
www.iddsi.org
There is also a helpful, free, IDDSI app available to download.
Useful Contact Information
Northern Health & Social Care Trust Speech & Language Therapy Services
In the NHSCT you can contact a Speech & Language Therapist directly, by calling the centre closest to you from the list below. You should ask for advice and discuss whether you might need a swallow assessment. The process in other Trust areas may be different.
Antrim Area Hospital
Tel: 028 9442 4442
Ballymena Health and Care Centre
Tel: 028 2563 5498
Moyle Hospital
Tel: 028 2826 6133
Mid Ulster Hospital, Magherafelt
Tel: 028 7936 6970
Fort Centre, Coleraine
Tel: 028 7034 7859
Whiteabbey Hospital
Tel: 028 9055 2328
Northern Health & Social Care Trust Dietetic Services
To request an appointment with a Registered Dietitian you will have to be referred to the service by a healthcare professional such as a GP, Consultant, Community Nurse or other Allied Health Professional.
MEAAP would like to thank our funders